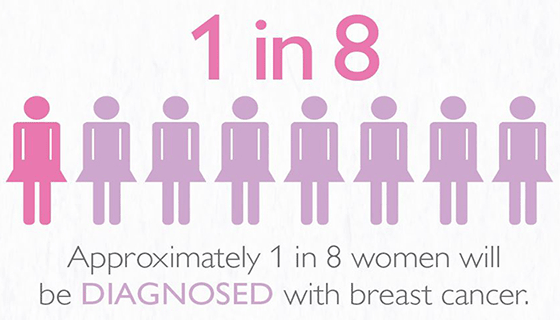
October is National Breast Cancer Awareness Month and, according to the World Cancer Research Foundation, 1 in 8 women will develop breast cancer within their lifetime. Events hosted this month will raise awareness about breast cancer and raise money for research. Here at Stevens, organizations host events like Breast Cancer Jeopardy, co-hosted on October 15 from 6 to 7 p.m. by the Lore-El Center and Colleges Against Cancer; the Making Strides breast cancer awareness walk on October 20 with Colleges Against Cancer; and the Bowling For Boobies fundraiser on October 25 from 5:30 to 10 p.m., hosted by Theta Phi Alpha and Delta Phi Epsilon. These opportunities are all great ways for students to get involved and support the cause. Stevens is also researching the cutting edge of treatment options for recurrent breast cancer.
In the Sharma Lab, named after its founder Dr. Abhishek Sharma, research is being done to discover and develop a new class of drugs for use in breast cancer treatment. 70 to 80% of breast cancers are caused by hormonal abnormalities, specifically in estrogens. Our cells contain estrogen receptors, which work to regulate and maintain healthy cell growth and division. Most of the time, estrogen receptors are in the “off” position and only activate when estradiol (also known as E2) binds to the receptor. You can think of this process as an on/off switch. When they are in the “off” position, the estrogen receptors do not activate cell growth or cause any other changes in the body. When the estrogen receptors are in the “on” position, they cause the cells to grow and divide.
Estrogen receptors are proteins, and all protein activities are regulated not just by the composition of the molecule, but also by its three-dimensional arrangement. Hydrogen bonding drives specific secondary and tertiary structures during polypeptide chain formation. When E2 comes into contact with an estrogen receptor, it shifts Helix 12, a specific portion of the tertiary structure of the protein, to the “on” position. This causes the protein to bind to the cell’s DNA and activate the gene which causes cell division. Cell division is necessary for healthy bodily function. However, when the estrogen receptors are overstimulated, uncontrollable cell growth occurs. These extra cells form a tumor, and cancer results.
Currently, there are two types of hormone therapies which work to combat tumor formation. The first therapy stops the production of E2. By decreasing the amount of E2 present in the cells, there is less stimulation of the estrogen receptor, so the excess cell division stops. Specific drugs which use this approach are Letrozole and Anastrozole, and they have both been on the market since 1996.
The second type of hormone therapy stops Helix 12 from shifting when the activator attaches to the estrogen receptor. These drugs, similar in structure to E2, bind the estrogen receptor as if they were E2. The difference comes in with the addition of a specific side chain which prevents the Helix 12 from shifting into the “on” position by physically getting in the way, a concept known as steric hindrance. Although there is still an overabundance of E2 in the blood, the presence of the drugs decreases the amount of “on” estrogen receptors and, therefore, slows cell division. Existing drugs for this type of therapy are Hydroxytamoxifene and Raloxifene, which were introduced in the late 1990s as well.
Although both of these hormone therapies are initially effective, they fail to treat recurring breast cancer. Sometimes, breast cancer returns 5 to 10 years after treatment. Often, hormone therapies which worked the first time are no longer effective because of mutations that have resulted in biological resistance. Recurring breast cancer is often metastatic, meaning it will spread to other parts of the body. Most commonly, breast cancers metastasize to the brain, chest wall, liver, lymph nodes, lungs, and/or bones. There are currently very limited treatment options for this type of cancer, and there have been no significant new types of treatments for almost 30 years.
This is the problem Dr. Sharma is working on in his lab. Dr. Sharma is developing a new class of compounds to decrease the
The development of the compounds Dr. Sharma is working on began in
The design of these molecules relies heavily on fundamental concepts in organic chemistry, physical organic chemistry, and medicinal chemistry. Most of these molecules possess complex structures and are constructed in Dr. Sharma’s lab from chemical building blocks using the techniques of synthetic organic chemistry. The chemical structure and purity of molecules obtained from these reactions are confirmed using analytical techniques such as Nuclear Magnetic Resonance (NMR) spectroscopy and mass spectrometry.
Working with a team of collaborators at Memorial Sloan Kettering Hospital and Scripps Research Institute Florida, these molecules are tested in various biological assays to evaluate their anti-cancer activity. The results from these assays are then used to further refine the design of drug candidates. This iterative cycle is repeated many times until a potent anti-cancer compound is identified for pre-clinical and clinical studies to ultimately provide a new treatment option for recurring and metastatic breast cancer.
According to Dr. Sharma, “We really want to use chemistry as a tool to develop novel drugs, and there is nothing more important for us than if we can use the tools and knowledge of chemistry to contribute to society. That’s the ultimate goal.”
Be First to Comment